What Are Massage Therapy Soap Notes
Health care professionals like massage therapists typically use SOAP notes to document and keep track of clients’ health records. SOAP is a special acronym that stands for the wordssubjective, objective, assessment, and plan. Over time, this type of note has become the standard for massage therapists to use in their practice, and they are critical for several reasons. They provide massage therapists a way to maintain a structured approach to their sessions and keep track of specific client information. This structure allows them to create outlines of their appointments to use the limited session time as effectively as possible to help their clients.
Are Soap Notes Required In A Yomassage Session
Yomassage always includes SOAP notes in their signature, table, and barefoot sessions, even if they are very basic or brief. However, these notes arent typically used during their Self-Care or Mindful Touch sessions. Yomassage covers how to create practical SOAP notes as part of the basic training courses for massage therapists, and they also have SOAP note sheets available via their membership portal. Therapists can access, , and use these note sheets at any time.
Related: Strengthening Your Massage Practice to Withstand Any Storm
Soap Notes For The Mblex
Here are a few key concepts about SOAP notes and written data collection to be sure to know for the MBLEx :
- What information belongs in a treatment note?
- Why is it important to document client sessions?
- Why is it important to measure and track progress towards goals?
- What is the difference between subjective and objective data
- You should include your clinical opinion in your documentation, but not your personal opinion or judgement.
You May Like: Brookstone Renew Zero Gravity Massage Chair Costco
Client Intake Forms Provide Consent
Sometimes these intake forms will provide a list of specific areas that your client needs to check off in order to provide consent for you to work on them. These are usually more sensitive places where not everyone feels comfortable being worked on.
Some examples of areas that require consent are the pectoral muscles, face, feet, scalp, glutes, and abdomen.
Are Our Massage Therapists Required To Keep Soap Notes
Keeping clinical documentation is an essential aspect of conducting a successful massage therapy service. SOAP notes document the treatment and progress of clients, improve communication, and are innovative tools when working with insurance companies.
Although other formats can assist with writing clinical notes, the SOAP structure is the most commonly used across professional modalities. Maintaining consistency and communication will improve the services offered by massage therapists, so keeping SOAP notes is highly recommended. Writing SOAP notes is not a requirement for some businesses and specific treatments, so checking the rules and regulations of the company you work for will be the best way to know what type of documentation you should be keeping. Often clinical documentation for massage businesses will be maintained using digital platforms that can improve efficiency and consistency.
Don’t Miss: Neck And Shoulder Massage Nyc
Why Is Documenting Important For Massage Therapists
Documenting client encounters is important for massage therapists for 4 main reasons:
If its not in writing, then it didnt happen.
Why Do Massage Therapists Use Soap Notes
Like other healthcare professionals, massage therapists use SOAP notes to detail: the treatment plan, the clients progress, new and substantial issues or pain, and notes for future treatment. They are also essential to making sure the therapist is updated before a clients visit and has a clear vision of the goals.
Recommended Reading: Can I Use Flex Spending For Massage
Advantages Of Soap Notes In Counseling
SOAP notes are great because they create a uniform system of your patients information. Without SOAP notes or other similar organized methods, every document would be different and difficult to quickly glance through for medical professionals. Here are some advantages of SOAP notes:
- SOAP notes are uniform system of tracking your patients information
- SOAP notes help other medical professionals thoroughly understand your patients issues
- SOAP notes help organize the most accurate information so that treatment can be the best possible
- SOAP notes adopt medical terms that most everyone in the medical field understands
Join Thousands Of Massage Therapists Saving Time With Massagebook
MassageBook electronically captures massage therapy session notes about your patients to help you track the treatment process and insurance billing. In addition to SOAP notes, this software is also a massage therapists one-stop-shop for marketing, website development, online scheduling, gift certificates, and more.
Want to see how MassageBook can help grow your practice? Create your Free account now, or get in touch with us to learn more.
Read Also: Best Massage Spa In Queens Ny
Common Abbreviations In Massage Therapy A Complete List
Abbreviations and acronyms are commonly used in all fields within the healthcare industry including massage therapy. Individual professions such as massage therapists, nurses, physicians, dentists and physical therapists tend to have their own set of abbreviations that they use most often. There are other abbreviations such as DOB, Dx, Hx, and SOAP that are consistently used across all health and wellness professions. It can be confusing, especially for new therapists, to remember the correct way to abbreviate commonly used terms when documenting or when reading another practitioners notes.
What are abbreviations? Abbreviations are a shortened form of commonly used words, terms or phrases. Abbreviations have been used in the medical field ever since the first medical texts, prescriptions and notes were written. This form of shorthand speeds up the written communication process, and may also involve the use of symbols.
This post was created as a guide to abbreviations for massage therapists. In this reference article, youll find a list of 200 of the most common abbreviations that massage therapists encounter in the course of performing their job, and may use when charting their client treatments.
Reminders To Create Soap Notes
Your day is packed. Youre booked back to back, and you just have enough time between clients to throw down a granola bar. How are you ever going to find the time to create proper notes? MassageBook keeps track of the clients youve worked on and provides a list of those who you have not yet created SOAP notes for. Just click on the client name, fill out the simple SOAP form, attach any documents you like, and click Save. Its that easy.
Also Check: What Is A Good Foot Massager For Plantar Fasciitis
What Is A Soap Note In Massage What Does Soap Stand For In Massage
Some of you might be wondering what a SOAP note even is.
SOAP notes are the formal documentation of your session. These are not to be confused with consent forms!
SOAP is an acronym that helps massage therapists structure their notes. While not everyone follows this format, its typically the industry standard.
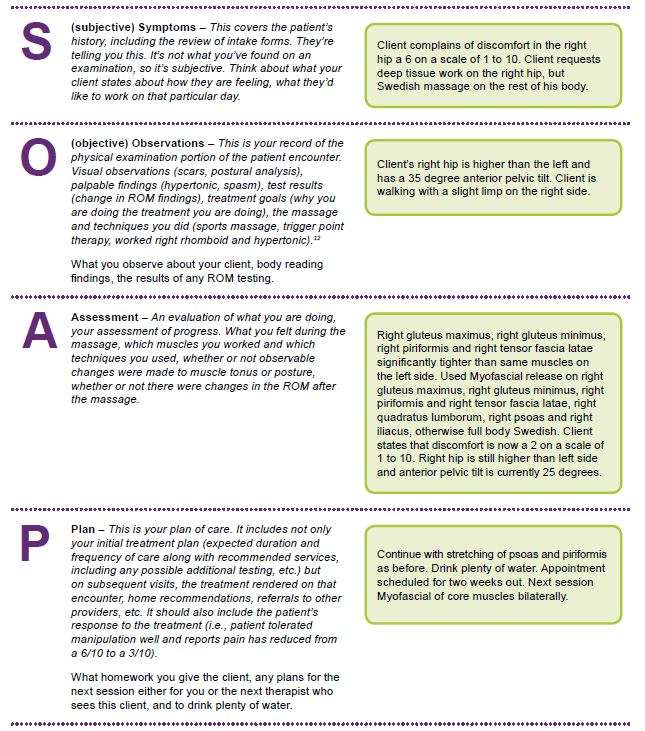
SOAP stands for the following:
S = Subjective: The clients description of their complaint. For example, the clients neck is sore. This section is completed before your session.
O = Objective: Your objective findings that are observable and/or measurable, both before and during the massage.
A = Assessment: How your client responded to the treatment. Its important to note that sometimes massage therapists will also include what areas they treated and the techniques used or if heat was used. In this way, there can be some discrepancy in how SOAP notes are taught .
P = Plan: The treatment plan for what you want to do in the future and recommendations for self-care.
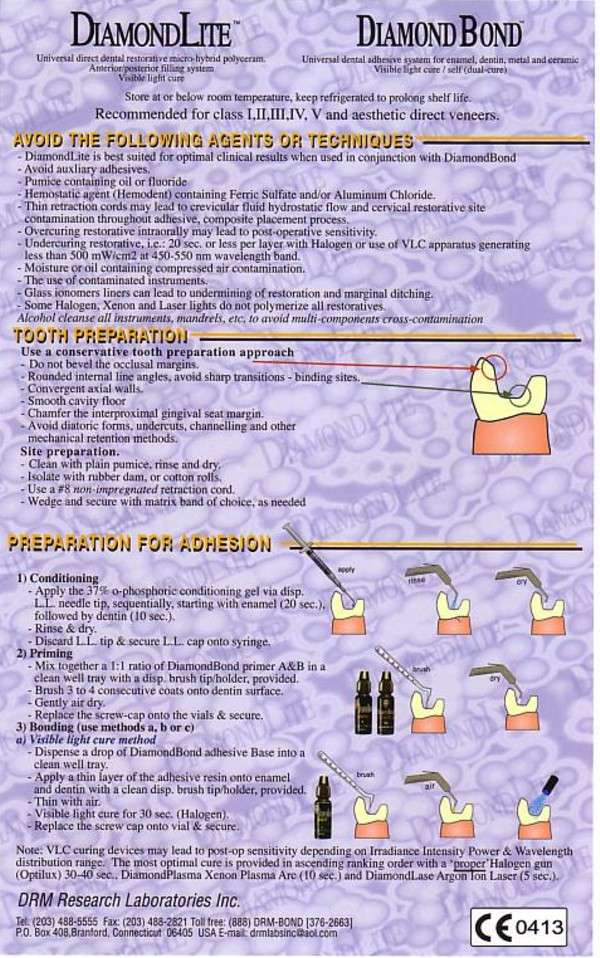
Soap Notes For Massage Therapy
SOAP is a method of documentation employed by health care providers including massage therapists to write out notes in a patients chart. A Massage Therapists duty is to assess and treat physical dysfunction and pain of the soft tissue and joints of the body and SOAP notes help in accomplishing this.
* If this is the patients first treatment visit, the massage therapist will get the patient to fill out a confidential Medical Health History Form. soap notes for massage therapy
You May Like: How To Advertise Massage Business
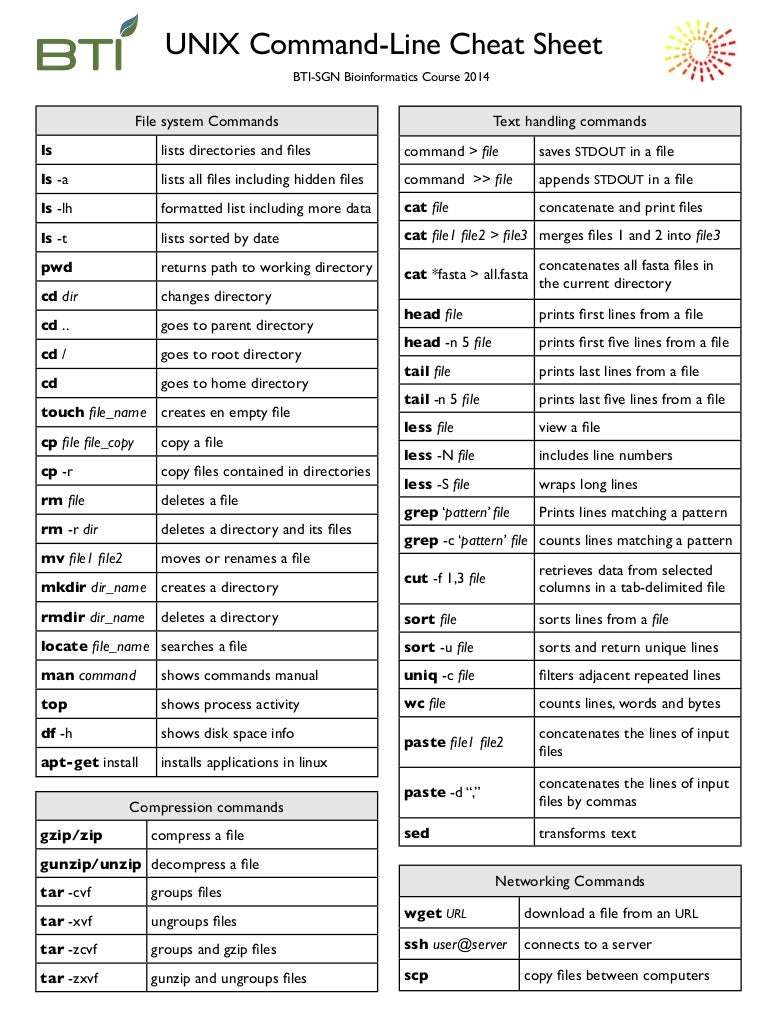
Recommended Massage Abbreviations And Symbols
The following table presents a list of abbreviations that massage therapists commonly use in their documentation. The abbreviations below are fairly standard, but your massage office may have a specific list of abbreviations that they want all clinicians to use in order to be more consistent, especially if you work at a medical or rehab clinic. The important thing is to be clear and be consistent.
| Abbreviation or Symbol |
|---|
Massage Therapy Soap Notes You Can Always Count On
Are paperwork headaches killing your productivity and workflow?
SOAP notes are not only a great way to keep track of your clients progress theyre required if youre considering doing any insurance billing. MassageBook SOAP notes are easy to use and seamlessly tied to each clients appointment records, making it easy to find past notes and create new ones. Theyre fully secure and HIPAA-compliant, so youll never have to worry about security issues.
You May Like: Green Mountain Chiropractic And Massage
What Goes In The Objective Section Of A Soap Note
The objective section of the SOAP note contains information that you gather through observation, palpation, or performing reassessment tests. This could include measuring range of motion , observing how a client walks, posture, affect, muscle tone, skin lesions, movement abnormalities, etc.
These are things that any other massage therapist would be able to observe if they were seeing the client. The objective section is often the most confusing section of SOAP notes for massage therapists.
What could go in the objective area of a SOAP note?
- Observations from assessment or reassessment, e.g. ROM, posture, etc.
- Progress towards goals, based on objective findings
- Details of specific treatments/modalities provided today. Include: position, techniques used, duration of treatment, areas of focus, equipment used
- Observable or palpable response to todays massage treatment
Common errors that massage therapists make in the objective section of a SOAP note:
- Vague information about treatments that were performed.
- Including value judgements, bias or personal opinions
- Inaccurate use of massage terminology
- Diagnosing based on observations. For example, Client demonstrated decreased left shoulder abduction ROM, indicating a frozen shoulder. Or writing this when a client does not have a diagnosis of muscle strain from physician: Client has pain at lower back due to muscle strain. A lower back muscle strain is a medical diagnosis .
Do what you write and write what you do.
What Are Soap Notes
SOAP notes are how massage therapists and other healthcare workers document their client sessions. The SOAP format provides clinicians an organized structure to document the most important parts of a client / patient encounter.
SOAP notes are a format for medical charting that have been around since the 1960s and it is currently one of the most widely used methods of documenting massage therapy sessions.
The basic format of the note follows the SOAP acronym:
S = Subjective. This section includes information that the client tells you in his or her own words.
O = Objective. Includes your clinical findings and observable data
A = Assessment. Your assessment or analysis of client response to treatment and progress towards goals.
P = Plan. Includes your plan for their next visit, and any instructions that you gave the client.
You will likely see dozens of variations of this SOAP note format, and different ideas about what information goes in each section. Some therapists use the SOAP note to document initial client evaluation. However from my experience, a separate eval form works better for that.
For example, the massage treatment you provide today usually goes in the objective section, even though it is very different information than objective data. The SOAP note examples provided by ABMP do it this way.
However other sources consider the A in SOAP to mean Assessment and Application, indicating this is where you include details of your massage treatment used today.
Read Also: Lower Back Pain Treatment Massage
Soap Note Template For Massage Therapists
- Amber Ludeman
- –
Running a successful massage therapy practice requires more than just dynamite technique. Organization and efficiency are essential to scheduling smoothly, marketing with impact and growing your business. Central to this organization is your clients paperwork. Not only do these documents direct your treatment plan and track progress, they can inform decisions made by insurance companies and other healthcare providers. This is why massage therapists rely on SOAP notes.
Add This Routine To Any Technique And Revolutionize Your Practice
As more Americans seek sessions from practitioners of integrative medicine, including massage therapists, the ethical, legal and professional obligations for thorough client health care records become more important.
Practitioners need accurate charts to keep track of a clients progress, support continuity of care within a health care team, document proof of service and avoid malpractice cases.
SOAP notes are an integral part of the vocation of massage therapy. Massage therapists rely on SOAP notes to help create long-term plans for client care, and insurance companies insist on them in order to process reimbursement.
In the case of a lawsuit, extremely organized, printed SOAP documentation will support the therapist. Comprehensive note-taking and features that prohibit the therapist from reopening and changing a note will help a therapist accused of malpractice. With electronic charting, SOAP notes are secure, date-stamped, legible and thorough.
With the passing of the Affordable Care Act , medical facilities and physicians are required to provide clients with electronic medical records . There are no formal requirements stipulated for massage therapists related to charting under the ACA however, that does not mean such charting will not be mandatory in the future.
Also Check: Mattress Firm Massage Chair Infinity
Purpose Of Soap Notes
Soap Notes Massage Tips
As a licensed or certified massage therapist, its essential to know about SOAP notesand how to properly and effectively record them as part of your sessions. SOAP notes will help you determine what you need to work on with your client as you go through the session. That way, you can make the time spent with them as effective as possible. It will also allow you to help establish a treatment plan for your client that can be used by other massage therapists going forward. This is everything you should know about recording useful SOAP notes as part of your sessions.
Related: The Power of Touch
Read Also: Sensual Massage With Essential Oils
Write Effective Massage Therapy Soap Notes + Examples
Updated on March 1, 2022 in practice management tips
Do you record SOAP Notes for each of your clients treatment sessions? SOAP Notes are a way for massage therapists and other healthcare providers to map where a client has been and where they are going. The unique SOAP format of these reports helps you keep track of your clients condition and progress through each treatment session.
And Why Are Soap Notes Important
SOAP notes give massage therapists a structured approach to help facilitate the most beneficial massage sessions for their clients.
Massage therapists know that every minute counts, so creating some sort of outline for your massage sessions will help utilize your time and your clients time in the most effective way.
Documenting SOAP notes can be an invaluable tool when dealing with insurance companies and it can also improve communication between you and your clients.
SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. Heres what they mean:
Don’t Miss: Massage Places In Gainesville Va
Massagebooks Basic Vs Premium Soap Notes
Both versions of MassageBooks SOAP notes are easy-to-use, allow you to save time and space, and are HIPAA-compliant. So whats the difference?
Basic SOAP Notes let you manually type your findings into each provided field: Subjective, Objective, Assessment, and Plan. This capability is included with all subscription plans.
Premium SOAP Notes expand on Basic by giving you the ability to add notes to the body chart using the auto-create and draw tools. These capabilities are only included with Simplify or Amplify pricing plans.
Basic SOAP note features:
- Reminders to create & update SOAP notes
- Mr. Meanie opens up
Premium SOAP note features:
- Visual markers with draw tool